Nobody should ever have to die of a highly preventable and treatable disease like cervical cancer. That’s why, not only for Cervical Cancer Prevention Week but year-round, we should strive to lift the veil of embarrassment regarding gynaecological health and keep the conversations flowing.
Knowing what symptoms to look out for and being able to make informed choices regarding preventative measures or treatment options could help save lives.
In the UK, over 21,000 people are diagnosed with one of the five gynaecological cancers each year, around 3,200 of which are cervical cancer cases. Thanks to advancements in both the cervical screening and HPV vaccination programmes, there has been an overall reduction in the disease in recent decades; rates have fallen by a quarter since the 1990s. Mortality rates for cervical cancer are also decreasing, down by three quarters since the 1970s.
On 17 November 2020, the World Health Organisation launched a historic first in their global strategy to accelerate the elimination of cervical cancer by improving accessibility to treatment for the disease. We already know how to prevent cervical cancer –screening prevents around 75 percent of cervical cancer cases. By 2030, WHO wants 90 percent of girls vaccinated against HPV, 70 percent of women screened for cervical cancer, and 90 percent of people with cervical disease to be given treatment. They hope these measures will lead to a worldwide cervical cancer-free future.
What is cervical screening?
The message has always been that the earlier any type of cancer is caught the better a person’s chances of treatment and survival will be. Prevention relies heavily on adequate screening which can help detect some cancers at an early stage. When caught in the pre-cancerous stages, cervical cancer is very treatable.
Cervical screening – or a smear test – is an internal test that detects first and foremost the common sexually transmitted human papillomavirus (HPV). It also looks for abnormal cells in the cervix that could later develop into cancer if left untreated.
Abnormalities are almost always (99.7 percent) caused by high-risk HPV. There are around 200 types of low and high-risk HPV and 80 percent of people will get one in their lifetime. HPV infects skin and moist membrane such as mucus in the cervix. Most people will have no problems. But persistent infection is what causes cells in the cervix to change.
While 13 types of HPV are linked to cancer, HPV detection doesn’t automatically mean you will get cancer. Cervical cancer is slow developing and can take between ten and 20 years for HPV to cause cell changes. Symptoms rarely occur for many years, unfortunately sometimes when it has metastasized (spread to other parts of the body). This is why screening is imperative.
Currently all women or people with a cervix who are registered with a GP and aged between 25-64 are automatically invited for regular smear tests every three or five years. If you have previously had a hysterectomy or pelvic radiotherapy which removed your cervix, you may be offered a vault smear to check the cells in your vagina are healthy.
There will always be two camps when it comes to screening invitations landing on the door mat: those who read it and forget about it (or choose to ignore it), and those who book an appointment straight away. Those in the former camp who put it off may do so out of the fear of the unknown, feeling embarrassed to go for screening, or having had a bad experience in the past. Often misconstrued, cervical screening is not a test for cancer. Perhaps thinking of the C-word fills many with dread.
And, yes, attending screening is a patient’s choice. But some patients may not be able to make an informed choice for many reasons – from lack of understanding, through to age, or inappropriate equipment. Cervical cancer rates are around 65 percent higher in the most deprived areas of the population; around 520 cases of cervical cancer each year in England are linked with deprivation.
Either way, lives are being put at risk by socioeconomic barriers to cancer screening.
Does the NHS always get it right with cervical screening?
Screening is not an infallible solution to cancer prevention, nor is it risk-free. Some patients may get an incorrect or misinterpreted result, such as a false positive or negative. This means they are either over-diagnosed and given unnecessary treatment, or have a late diagnosis when their cancer has advanced and curative treatment options have dwindled. However, if undertaken correctly and without error or negligence, the benefits of having a smear test far outweigh the risks.
But if a patient has been having regular screening and is then diagnosed with late-stage cervical cancer, questions need to be asked.
Too often our solicitors witness the tragic results of medical errors, particularly regarding women’s health. When you put your life in the hands of medical experts, you expect you will be listened to, cared for and given the best treatment possible. Women should feel confident in speaking to medical professionals about their bodies.
Yet we continue to hear of stories in the news where gynaecological cancers are occurring due to medical errors or lack of understanding regarding the female reproductive system. People whose crippling symptoms of uterine cancer are being mistaken for digestive disorders. Women forced to pay for private gynaecology appointments after being refused referrals by their GP, only to discover large tumours in the pelvis. Those who fall under the minimum screening age dying before their 25th birthday after symptoms were downplayed as ‘normal’ side effects of contraception or hormones. Pregnant women who have been told they’ve got cervical cancer having to choose between prolonging their own life or giving life to their unborn child.
What accounts to cervical cancer negligence?
Mistakes in diagnosing gynaecological cancers can be very serious, but the success of a negligence claim is contingent on whether you can prove that such delay affected the outcome. Simply put: would you have had a better result and less extensive treatment if your cancer had been diagnosed and treated earlier.
Treatment options for cervical cancer can be very aggressive, even if a patient is diagnosed at an early stage. You may be offered a trachelectomy if your tumour is 2cm, a procedure which doesn’t remove the womb. But many will be given a hysterectomy. For a woman of child-bearing age, side-effects affecting fertility can be physically and emotionally difficult to comprehend, more so if diagnosis is as a result of avoidable delays.
At Medical Solicitors, our team have worked with people who have been affected by delayed or wrong diagnosis of gynaecological cancers, particularly cancer of the cervix. Some of the lasting effects they experienced due to incorrectly interpreted smear tests include lymphadenopathy of the legs caused by a radical hysterectomy, permanent nerve damage during surgery to remove the womb, reduced life expectancy by almost four decades, and avoidable hysterectomies – all of which could have been prevented had their cervical histology (examination of tissue samples) been reported accurately and the correct treatment started earlier.
Examples of gynaecological cancer negligence include:
- Failure to carry out an adequate examination or take an accurate history
- Failure to refer a patient to a gynaecological oncologist for further investigation
- Mistakes in interpreting smear tests
- Mistaken diagnosis of cervical cancer often resulting in unnecessary surgery
If you are diagnosed with abnormal cells or cervical cancer, you should discuss with your physician the treatment options available to you, the risks and benefits of each, and any side effects such as fertility issues. Depending on the stage your cancer is found, there may be options to preserve your fertility. A landmark ruling at UK Supreme Court recently ruled the NHS can be ordered to pay for surrogacy treatment abroad if a hospital’s negligence leaves a woman infertile.
Screening in the coronavirus pandemic
With Covid-19 cases rising and the NHS overwhelmed, people are bound to feel more worried about visiting their GP for their routine screening appointments or to address any symptoms they may be experiencing. But your gynaecological health should remain a priority.
Screening programmes are now back up and running, however some NHS trusts are seeing delays with results taking longer than four weeks to get back to patients due to the influx of Covid tests they are undertaking. If HPV is found but no cells have changed, you’ll be asked to return in 12 months to see if the virus has gone. If abnormal cells are found, you should be sent for more tests including a colposcopy – some of which are also being delayed due to Covid.
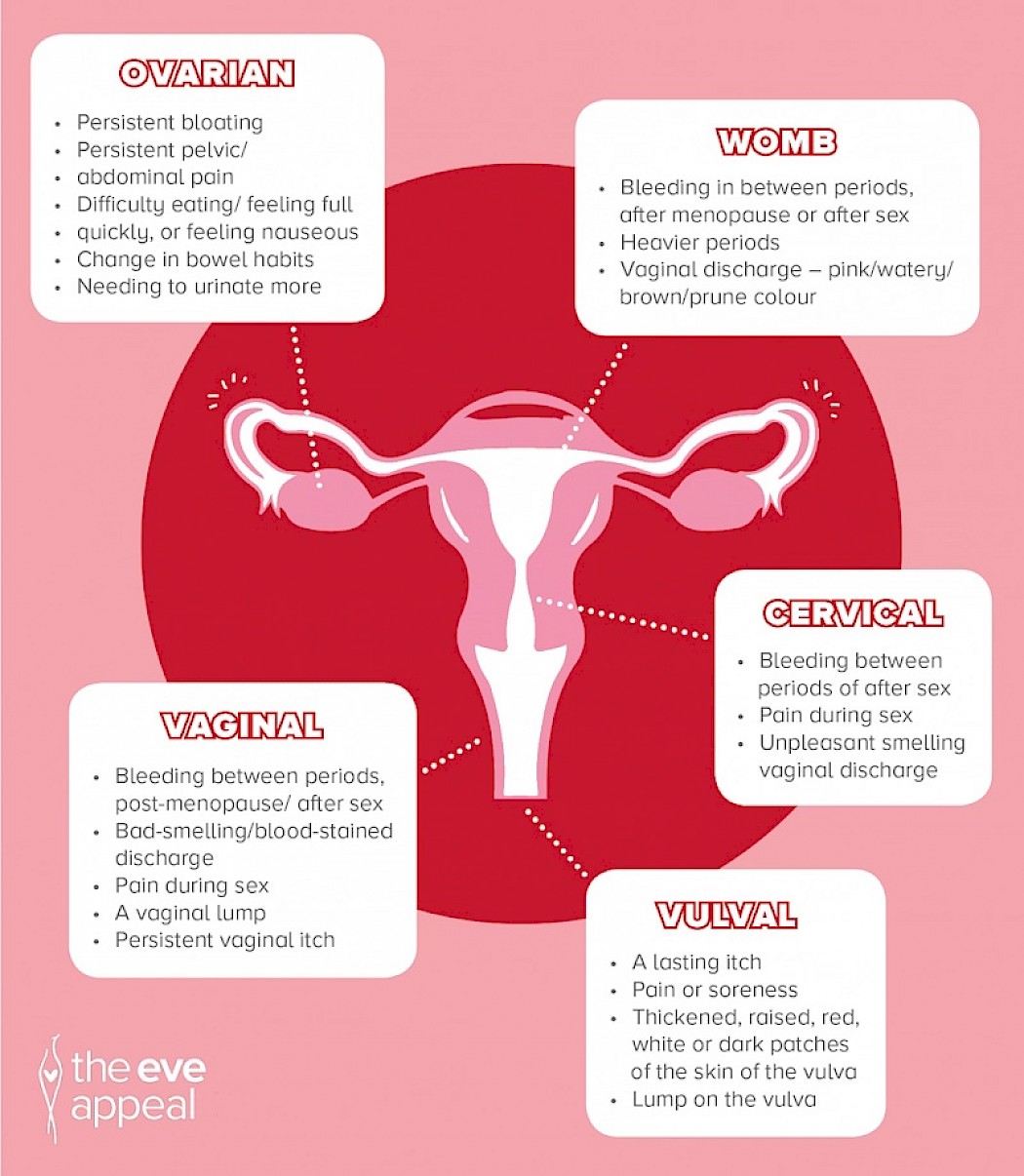
Unfortunately, there currently aren’t any routine screening programmes for the other four gynaecological cancers: uterine, ovarian, vaginal and vulval. Yet many of these, particularly ovarian cancer, are diagnosed late. Ovarian cancer is the biggest killer of all the gynaecological cancers and can be genetic; however, a new breakthrough drug called niraparib has recently been approved, increasing the likelihood of prolonging the lives of thousands of women diagnosed at a later stage. Uterine (or womb) cancer is the most common, especially in post-menopausal women, and cases have risen over 50 percent since the ‘90s. Vaginal and vulval cancers can be caused by HPV too, and you may be more at risk of vaginal cancer if you have had abnormal cells detected. Some symptoms of gynaecological cancers may be difficult to detect due to their non-specific nature. If you have any symptoms that are unusual for you, keep pushing for answers.
This is a great infographic by The Eve Appeal which highlights the symptoms of each gynae cancer:
If you have any concerns or questions about the impact of screening, diagnosis or treatment during the pandemic, The Eve Appeal has great Gynaecological Cancer resources that may be able to help.
A cervical cancer-free future?
The HPV vaccination programme currently being offered to year eight secondary school pupils in the UK plays a central role in reducing future cervical cancer cases. Offered to both girls and boys aged between 12-13 (or 11-12 in Scotland), it protects against four strains of HPV and lasts for a minimum of ten years. However, on reaching their 25th birthday, pupils who received the vaccine as a teenager should still attend their smear tests when invited. It is not an immunity pass. With disruption in schools due to Covid-19, some parents may worry that their child will miss their HPV jab. But if an adolescent was offered it and missed/declined it for any reason, they are still eligible to have it on the NHS free of charge until they are 25.
One of the most important ways we can work towards eradicating cervical cancer is to talk. Talk to your mothers, sisters, daughters, relatives, friends and colleagues about your gynae health. Don’t feel uncomfortable to ask questions. If they talk about any symptoms they may be having, give them a gentle nudge to seek medical advice. If you know someone close to you is approaching 25 or has not yet had their first smear, talk about your own experience to help dispel any myths or worries they may have. Encourage people not already registered at a GP to do so to ensure they receive screening invitations.
This January, join the #SmearforSmear campaign and help raise awareness of ways to prevent cervical cancer. Not only could you save lives, but sharing stories could help save people from feeling alone if they are diagnosed with gynaecological cancer or undergoing treatment. Jo’s Trust has a brilliant comprehensive collection of resources and information regarding the cervix, HPV, screening and treatment, along with support services.
At Medical Solicitors, we’ll continue to advocate for improvements in women’s medical care and fight the corner for those affected by substandard care. Cancer screening is paramount to preserving and protecting our health and we are fortunate in the UK to have access to such indispensable programmes. But when inaccuracies occur, those consequentially affected may need support to rebuild their lives. We are here for you when you need it the most.

